Obsessive-Compulsive Disorder
Dealing with OCD
Research suggests that cognitive-behavioural approaches (e.g. CBT) are most likely to be helpful.
One particularly effective technique is called ‘Exposure and Response Prevention’, or ‘ERP’ for short.
Exposure and response prevention
The first step in ERP is to develop an anxiety hierarchy. There’s an example below. The number in the right-hand column refers to the amount of distress you feel when exposed to the trigger, on a scale of ‘0’ to ‘100’. These ratings are called Subjective Units of Distress, or ‘SUDS’ for short.
Each item on the hierarchy is more challenging than the one before it.
Make your own table to identify your own triggers in order of distress, then rate their SUDS.
The second stage of ERP is to learn an effective way of soothing yourself.
Self-soothing
Before we begin tackling the ‘triggers’ on your hierarchy, it’s important to find a way to calm yourself. Slow, measured breathing can help. Try the following exercise and practice until it becomes second nature.
Self-soothing by slowing the breath
- Place the flat of your hand over your stomach
- Open your mouth and breathe out with a sighing sound. As you breathe out, allow your shoulders and upper body muscles to relax
- Close your mouth and pause. Keep your mouth closed and breathe in through your nose; your stomach should move out as you breathe in
- If your shoulders rise again or your stomach doesn’t move out, slow down and try again till you’re breathing by pushing your stomach out
- Breathe out slowly, gently and deeply
- Repeat steps 3 – 4 – 5 until you feel more calm
Breathing by pushing out your stomach means you’re using your diaphragm to breathe – that’s the large muscle underneath your lungs. This helps us breathe more deeply and can help restore calm.
You might find you’re taking in a bit more oxygen like this, so might feel a little light-headed. This is nothing to worry about, just slow your breathing if this is the case.
Self-soothing using the five senses
Effective self-soothing can involve one or more of the five senses (sight, sound, smell, taste, and touch). Below are examples of self-soothing strategies for each sense.
When self-soothing, focus completely on the task. Be mindful of your senses and what you are experiencing. When you notice yourself becoming distracted (we always get distracted), gently bring your attention back to self-soothing.
- Go for a walk, notice beautiful things. Go to a museum with beautiful art. Buy or gather flowers. Sit in a garden. Light a candle and watch the flame. Look at a book with beautiful scenery or beautiful art.
- Listen to beautiful or soothing music, to tapes of the ocean or nature sounds. Listen to children laughing, birds singing. Sit by a waterfall. As you are listening, notice the sounds, simply let them come and go.
- Smell food being cooked. Walk in a garden or in the woods, maybe just after a shower of rain, breathe in the smells of nature. Light a scented candle or incense. Wear scent or cologne. Bake bread, make fresh coffee.
- Eat a special treat slowly, savour each bite. Cook a favourite meal. Drink a soothing drink, maybe herbal tea or hot chocolate. Let the taste linger on your tongue and pass slowly down your throat.
- Take a bubble bath. Pet your dog or cat, or cuddle a baby. Put on soft clothes. Take a hot or cold shower. Have a massage. Sink into a comfortable bed. Float or swim in a pool, feel the water caress your body.
Identify your own self-soothing strategies that feel right for you. The more you can come up with, the more you’ll be able to restore your calm. Practice self-soothing each day to help ‘train’ your autonomic nervous system to relax.
Once you have identified your trigger hierarchy and have found a reliable way to soothe yourself, begin exposing yourself to the items on your list. Start with those which are least distressing.
‘Exposure’ means deliberately doing the things that are distressing – touching ‘contaminated’ objects, deliberately thinking disturbing thoughts, maybe leaving things unfinished, or out of order or alignment.
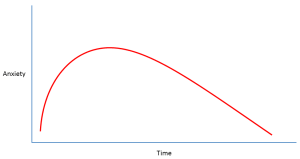
Don’t try to distract yourself from the anxiety this will cause. Over a period of time your anxiety levels will reduce. The key is not to ‘zone out’, not to avoid the trigger and not to perform any anxiety-lowering rituals. Just stay with the distress and practice slow, calm breathing until your anxiety reduces by at least half. If your SUDS was 80 to begin with, stay with the trigger until your SUDS is less than 40.
Nobody can remain anxious forever – over time a process of ‘habituation’ occurs where the trigger will become less distressing. Expect to experience high levels of anxiety when you first do the exposure, this will come down with practice.
You might want to have someone with you at first, but the goal is to be able to face the trigger just by yourself, with no compulsions, no emotional ‘crutches’ and no running away. Practice each item on your hierarchy until it causes little or no distress before moving onto the next, more challenging item.
The following chart shows how, if we stay with the distress, without avoiding, neutralising or engaging on obsessions or compulsions, anxiety diminishes over time.
ERP can be challenging to carry out on your own. Some people find it’s easier to get help from a trained professional, who can help with trigger hierarchies and with extra help and support.
Professional help
Your first appointment with a professional can feel difficult, especially if you feel uncomfortable, embarrassed or ashamed. Many people find it helpful to write down what you want to talk about before they meet. Make a note of any questions or worries you might have. Some people find it helpful to take a friend or family member along.
Sometimes it can be hard to summon the courage to get help. A simple ‘phone call to your GP can get things moving and start you on the road to recovery.
Avoid avoiding
Sometimes we just want to shut ourselves away from people. It can be very hard, but keeping active and staying with people can be very helpful. Remaining in work or returning to work might be very hard too, but can help us keep a sense of control. Keeping a normal daily routine is usually much better than withdrawing and staying in bed. We might feel like shutting ourselves away, but doing so can make things worse.
Ask yourself, ‘if there’s something I’m avoiding, what could I do differently? Make a note of your answer.
Deal with the difficult things
Putting off problems can make them mount up. Are there things in your life you’re putting off dealing with? Might an advocate or some extra support help? The Citizens Advice Bureau can help with a range of issues from housing to money worries. Doing things to address our problems relieves the burden and makes us feel ‘in control’ again.
Ask yourself, ‘what small thing could I do today that would help me begin to feel better about myself?’ Make a note of your answer.
Avoiding alcohol and drugs
Alcohol is a depressant – it lowers the mood. Other non-prescribed drugs can have similar effects and are best avoided. If you think alcohol or drug use might be a problem, you can contact DAN 24/7, the Wales Drug and Alcohol Helpline: DAN 24/7 website or call them on 0808 808 2234.
Self-help resources
There are many good books and websites that can help. Again your GP, practice nurse or primary care mental health practitioner will be able to recommend from a range of excellent and helpful material. Some of the material in this information sheet has come from OCD-UK (http://www.ocduk.org/), a leading national charity for children and adults whose lives are affected by OCD.
Act now!
The sooner you get the help you may need, the sooner you’ll feel better! Speak with your GP or a health professional for extra information or to get on the road to recovery today!
Y-BOCS
The Yale-Brown obsessive-compulsive symptom checklist (Y-BOCS) is widely used by professionals to assess obsessions and compulsions. Below is a shortened version. Rate your current obsessions on a scale from ‘0’ to ‘100’ as to how much discomfort they cause, where ‘0’ represents no discomfort and ‘100’ represents extreme panic. You can also add any details that you think are relevant, such as the specific nature of a fear or obsession.
Avoidance
What objects, activities or situations do you avoid because of your obsessions? Make a list and rate each item on a scale from ‘0’ to ‘100’ as to how comfortable it would be to confront it, where ‘0’ represents no discomfort and ‘100’ represents extreme panic.
Compulsions
Compulsions (or rituals) are actions repeated to reduce discomfort (e.g. anxiety or guilt) which one feels driven to perform. Rate your current compulsions on a scale from ‘0’ to ‘100’ as to how much discomfort would occur if you were unable to perform them, where ‘0’ represents no discomfort, and ‘100’ is extreme panic.
Helping Agencies
You can find a list of national agencies that can help with OCD here: National OCD Agencies
Disclaimer
This material is for information only and should not be used for the diagnosis or treatment of medical conditions. We have used all reasonable care in compiling the information but make no warranty as to its accuracy. We recommend you consult a doctor or other health care professional for the diagnosis and treatment of medical conditions, or if you are at all concerned about your health.